A study published September 25 in the journal Nature Mental Health found that the brains of those with a substance use disorder have a connected circuit, giving researchers some potential places to target in future clinical treatments.
According to the United States Substance Abuse and Mental Health Services Administration, substance use disorders occur when someone’s recurrent use of alcohol and/or drugs causes them significant health problems, including “Disability, and failure to meet major responsibilities at work, school, or home.” In the United States, more than 20 million individuals are estimated to have substance use disorders and some common disorders are opioid use disorder, nicotine use disorder, and alcohol use disorder.
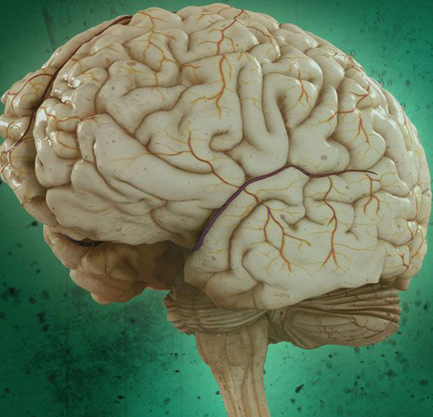
Brain scans or neuroimaging can help inform treatment options, since abnormalities in brain scans are associated with substance use disorders.
Some newly developed approaches to study the brain’s role in addiction include a process called brain lesion network mapping.
Brain lesions are areas of brain tissue that show damage from injury or disease.
“We can think of that as an average wiring diagram of the human brain in order to show how two lesions in two different sites that both cause the same issue actually share connectivity to the same region,” study co-author and University of British Columbia medical student Jacob Stubbs tells PopSci.
There are multiple ways to study brain imaging, which can make looking at the data even more complicated and noisy. A 2022 study mapped brain lesions to a circuit in the brain that can actually make the lesions go away in the brains of some cigarette smokers. This new study used that data to evaluate this newly discovered brain circuit and areas where the brain had atrophied, or shrunk. It evaluated data from 144 studies on addiction and found that abnormalities across substance use disorder are in a common brain network.
“Our study found that different brain regions implicated in addiction are all a part of a common brain circuit,” study co-author Michael Fox, founding director of the Center for Brain Circuit Therapeutics at Brigham and Women’s Hospital, said in a statement.
“Consistency across different papers means we now have a brain circuit to target addiction with treatments, rather than just a region.” The team reviewed data involving more than 9,000 participants.
The newly uncovered connection suggests a potential brain circuit that could be targeted neurostimulation therapies to treat substance use disorders.
“The five regions that pop up are places that actually do make some amount of intuitive sense. The medial prefrontal cortex is the strip of cortex that goes right down the front of your brain and it’s important because it’s been a target for successful neurostimulation trials,” says Stubbs.
