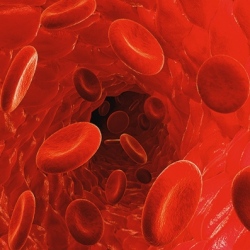
European scientists have found a way to convert skin cells into red blood cells, potentially clearing a path to make blood transfusions much safer because blood could have a patient’s own genetic code. Cells within the body – brain, muscle, fat, bone and skin – share that same code.
It makes sense that if unhealthy cells need to be replaced, they should be replaced from within the patients’ own body. "Convincing" skin cells to become red blood cells, however, is just as difficult as it sounds.
Enter researchers at Lund University in Sweden and the Center of Regenerative Medicine in Barcelona, who with the help of a retrovirus have identified the four genetic keys that unlock the genetic code of skin cells and reprogram them to start producing red blood cells.
"This is the first time anyone has ever succeeded in transforming skin cells into red blood cells, which is incredibly exciting," said Sandra Capellera, a doctoral student and lead author of the study.
Using the retrovirus, the team introduced various combinations of over 60 genes into skin cells’ genome, until they finally found the formula to change skin cells into red blood cells.
The study, published in the scientific journal Cell Reports, showed that just four of 20,000 genes are necessary to reprogram skin cells and have them start producing red blood cells – all four are necessary for the method to be successful.
"It’s a bit like a treasure chest where you have to turn four separate keys simultaneously in order for the chest to open," explained Capellera.
Johan Flygare, manager of the research group and in charge of the study, said: "We have performed this experiment on mice, and the preliminary results indicate that it is also possible to reprogram skin cells from humans into red blood cells. One possible application for this technique is to make personalized red blood cells for blood transfusions, but this is still far from becoming a clinical reality."
There would need to be significant investigation into how the newly created blood performs in living organisms. However, the significance of any clinical could be huge.
Flygare explained that: "An aging population means more blood transfusions in the future. There will also be an increasing amount of people coming from other countries with rare blood types, which means that we will not always have blood to offer them."
Patients with anaemic diseases could benefit in particular. It’s condition in which the patient has an insufficient amount of red blood cells, millions suffer worldwide, and there is a shortage of donors. The amount of blood patients need to receive from different donors means they can eventually have allergic reactions to new blood. Making new blood from their own bodies would remove this problem entirely.
