In a study published today in Science Translational Medicine, a team from Merck Research Laboratories reports results of early human and animal trials of a drug called verubecestat, which targets the production of protein plaques associated with the disease.
“It’s a summary of the discovery and early-stage profiling of what we hope is going to be a new therapeutic for Alzheimer’s,” says team leader Matthew Kennedy. “It represents well over a decade of investment in this project by many, many scientists.” Definitive conclusions will have to await the results of larger, ongoing phase III clinical trials to assess their efficacy, effectiveness and safety, but the results are promising, experts say.
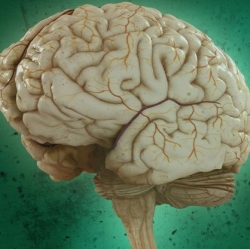
Verubecestat is a so-called BACE1 inhibitor. BACE1 (for Beta-site Amyloid precursor protein Cleaving Enzyme 1, aka beta-secretase 1) is an enzyme involved in producing amyloid beta, a protein that clumps together, eventually forming the plaques surrounding neurons that are the disease’s key hallmark. The amyloid hypothesis of Alzheimer’s proposes that the accumulation of amyloid beta aggregates in the brain drives a cascade of biological events leading to neurodegeneration.
By blocking BACE1, the hope is this approach could prevent the buildup of these clumps in the first place. But until now, development of these drugs has been hindered by problems finding molecules with the right characteristics, and concerns over theoretical and actual side effects. .
Amyloid is formed when amyloid precursor protein (APP) is cleaved into pieces by BACE1 and another enzyme called gamma-secretase. APP protrudes from cell membranes into the space between cells, where the enzymes can cut it. Production of amyloid beta involves two snips.
First, BACE1 cleaves it some distance from the cell (producing fragments called sAPP beta) then gamma-secretase cuts the remaining stub off at the cell membrane. The fragment released by this cut is amyloid beta. BACE1 inhibitors work by attaching to the enzyme and preventing it from cleaving APP, thereby decreasing production of amyloid.
BACE1 was discovered in 1999 by a team led by molecular biologist Robert Vassar, now at Northwestern University, who was not part of this study. Researchers have been studying its function using mice engineered to lack the BACE1 gene, and these studies have revealed numerous consequences including problems with insulation and guidance of neural wiring, retinal pathology and neurodegeneration, raising concerns that BACE1 inhibitor drugs might have side effects.
Another challenge was developing molecules big enough to attach to BACE1 but still able to cross the blood–brain barrier. Several candidate drugs have now been developed, but a recent clinical trial was halted due to evidence of liver toxicity.
The Merck team has developed a molecule that appears to overcome these challenges. They tested the drug on animals and found it significantly reduced levels of both amyloid and sAPP beta in the blood, cerebrospinal fluid and brain in a dose-dependent manner. There were no signs of toxicity, even after treatment of up to six months in rats and nine months in monkeys. The only obvious side effect was reduced fur pigmentation in mice and rabbits, although this wasn’t seen in monkeys.
The researchers then moved on to small, early-stage human trials to assess safety and tolerability and inform the choice of suitable doses for later trials. Verubecestat reduced amyloid and sAPP beta in the cerebrospinal fluid of healthy adults who took the drug for two weeks and patients with mild to moderate Alzheimer’s who took it for one week. “This is the first detailed report of what a BACE inhibitor does in humans,” says Dennis Selkoe of Harvard University, a leading Alzheimer’s researcher who was not involved in the work. “The good news is they didn’t see evidence so far of any of the side effects we’re concerned about with BACE inhibition.”
