Researchers have discovered a powerful type of immune cell in the meninges (covering) of the brain that are activated in response to central nervous system injury, suggesting that these cells play a critical role in supporting healthy mental functioning.
By harnessing the power of the cells, known as “type 2 innate lymphocytes” (ILC2s), doctors may be able to develop new treatments for neurological diseases, traumatic brain injury, and spinal cord injuries, as well as migraines, the researchers suggest. They also suspect the cells may be the missing link connecting the brain and the microbiota in our guts, a relationship that has been shown to be important in the development of Parkinson’s disease.
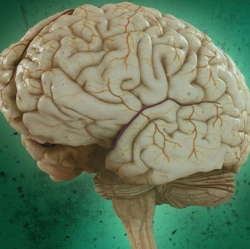
ILC2 cells have previously been found in the gut, lung, and skin, the body’s barriers to disease. Their discovery by UVA researcher Jonathan Kipnis, PhD, in the meninges, the membranes surrounding the brain, comes as a surprise. They were found along the same vessels discovered by the Kipnis lab last year, which showed that the brain and the immune system are directly connected.
“This all comes down to immune system and brain interaction,” said Kipnis, chairman of UVA’s Department of Neuroscience. These where previously believed to be not communicating, but not only are these [immune] cells present in the areas near the brain, they are integral to its function, Kipnis said.
Immune cells play several important roles within the body, including guarding against pathogens, triggering allergic reactions, and responding to spinal cord injuries. But its their role in the gut that makes Kipnis suspect they may also be serving as a vital communicator between the brain’s immune response and our microbiomes (microbes in the body). That could be very important, because our intestinal flora is critical for maintaining our health and well being.
“These cells are potentially the mediator between the gut and the brain. They are the main responder to microbiota changes in the gut,” Kipnis said. “They may go from the gut to the brain, or they may just produce something that will impact those cells. We know the brain responds to things happening in the gut. Is it logical that these will be the cells that connect the two? Potentially.”
The findings have been published online by the Journal of Experimental Medicine. The work was supported by a National Institutes of Health grant.
