Scientists have used chemicals to transform skin cells into heart and brain cells, instead of adding genes, making this a breakthrough, according to the scientists. The research lays the groundwork for being able to regenerate lost or damaged cells directly with drugs.
Instead, in two studies published in an open-access paper in Science and in Cell Stem Cell, the team of scientists at the Roddenberry Center for Stem Cell Biology and Medicine at Gladstone used chemical cocktails to gradually coax skin cells to change into organ-specific stem-cell-like cells and ultimately into heart or brain cells.
“This method brings us closer to being able to generate new cells at the site of injury in patients,” said Gladstone senior investigator Sheng Ding, PhD, the senior author on both studies. “Our hope is to one day treat diseases like heart failure or Parkinson’s disease with drugs that help the heart and brain regenerate damaged areas from their own existing tissue cells. This process is much closer to the natural regeneration that happens in animals like newts and salamanders, which has long fascinated us.”
Transplanted adult heart cells do not survive or integrate properly into the heart and few stem cells can be coaxed into becoming heart cells. Instead, in the Science study, the researchers used a cocktail of nine chemicals to change human skin cells into beating heart cells. By trial and error, they found the best combination of chemicals to begin the process by changing the cells into a state resembling multipotent stem cells (cells that can turn into many different types of cells in a particular organ). A second cocktail of chemicals and growth factors then helped transition the cells to become heart muscle cells.
With this method, more than 97% of the cells began beating, a characteristic of fully developed, healthy heart cells. The cells also responded appropriately to hormones, and molecularly, they resembled heart muscle cells, not skin cells. What’s more, when the cells were transplanted into a mouse heart early in the process, they developed into healthy-looking heart muscle cells within the organ.
“The ultimate goal in treating heart failure is a robust, reliable way for the heart to create new muscle cells,” said Srivastava, co-senior author on the Science paper. “Reprogramming a patient’s own cells could provide the safest and most efficient way to regenerate dying or diseased heart muscle.”
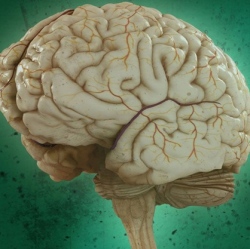
With their improved safety, these neural stem-cell-like cells could one day be used for cell replacement therapy in neurodegenerative diseases like Parkinson’s disease and Alzheimer’s disease, according to co-senior author Yadong Huang, MD, PhD, a senior investigator at Gladstone. “In the future, we could even imagine treating patients with a drug cocktail that acts on the brain or spinal cord, rejuvenating cells in the brain in real time.”
