Scientists have found a way to change leukemia cells into leukemia-killing immune cells. The surprise finding could lead to a powerful new therapy for leukemia and possibly other cancers as well. "It’s a totally new approach to cancer, and we’re working to test it in human patients as soon as possible."
The Lerner laboratory has pioneered techniques to generate and screen very large libraries of antibodies (immune system molecules), using the power of large numbers to find therapeutic antibodies that bind to a desired target or activate a desired receptor on cells.
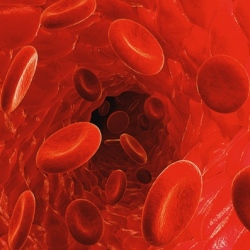
Recently, the lab mounted an effort to find therapies for people with certain immune cell or blood factor deficiencies, by looking for antibodies that activate growth-factor receptors on immature bone marrow cells that might induce these bone marrow cells to mature into specific blood cell types. Over the past few years, Lerner and his team succeeded in identifying a number of antibodies that activate marrow-cell receptors in this way.
In the process, the scientists noted that some of these receptor-activating antibodies have unexpected effects on marrow cells, causing them to mature into radically different cell types, such as neural cells. While why this happens is an unresolved issue, the discovery led the team to wonder if they could also use the method to convert cancerous marrow cells (leukemia cells) into non-cancerous cells.
To find out, in the new study Lerner and his team, including first author Kyungmoo Yea, an assistant professor of cellular and molecular biology at TSRI, tested 20 of their recently discovered receptor-activating antibodies against acute myeloid leukemia cells from human patients. One of these antibodies turned out to have an extraordinary impact on the acute myeloid leukemia cells.
A high percentage of acute myeloid leukemia cells express the thrombopoietin (TPO) receptor, and the effective antibody was a highly potent and selective activator of this receptor on marrow cells. When the antibody was applied to healthy immature marrow cells, it caused them to mature into blood-platelet-producing cells called megakaryocytes. However, when the antibody was applied to acute myeloid leukemia cells, they matured into very different cells known as dendritic cells, key support cells in the immune system.
By itself, this could be a valuable therapeutic strategy, but it wasn’t the end of the story. Lerner’s team noted that, with longer exposures to the antibodies and certain other lab-dish conditions, the induced dendritic cells developed further, into cells that closely resembled natural killer (NK) cells.
NK cells represent one of the rapid-reaction forces of the immune system. They can be effective against viruses and bacteria, and cancer cells, even without prior exposure. They don’t have highly specific receptors for recognizing individual targets, as T-cells do, but instead are capable of detecting, in a general way, when a nearby cell is infected or cancerous.
"That antibody could have turned those acute myeloid leukemia cells into a lot of other cell types, but somehow we were lucky enough to get NK cells," Lerner said.
