New research suggests that psilocybin-assisted therapy helps alleviate treatment-resistant depression by reviving emotional responsiveness in the brain. Psilocybin is the primary mind-altering substance in psychedelic “magic” mushrooms.
The drug can profoundly alter the way a person experiences the world by producing changes in mood, sensory perception, time perception, and sense of self.
The new study, published in the scientific journal Neuropharmacology, found that depressed people had increased neural responses to fearful faces one day after a psilocybin-assisted therapy session, which positively predicted positive clinical outcomes.
“I believe that psychedelics hold a potential to cure deep psychological wounds, and I believe that by investigating their neuropsychopharmacological mechanism, we can learn to understand this potential,” explained study author Leor Roseman, a PhD student at Imperial College London.
For the study, 20 patients with major depression underwent two psilocybin-assisted therapy sessions. The participants received fMRI brain scans before their first session and on the morning after their second session.
While receiving the brain scans, the participants viewed images of faces with fearful, happy, and neutral expressions.
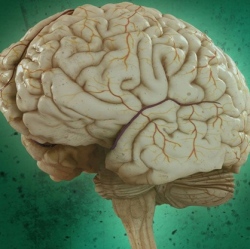
The researchers were particularly interested in a brain structure known as the amygdala, which is associated with emotional processing and threat detection.
Following the psilocybin-assisted therapy sessions, the majority of patients reported that the treatment improved their depressive symptoms.
Roseman and his colleagues observed heightened amygdala responses to both fearful and happy faces after treatment with psilocybin. However, only increased amygdala responses to fearful faces were associated with successful clinical outcomes one week later.
“Psilocybin-assisted therapy might mitigate depression by increasing emotional connection, this is unlike SSRI antidepressants which are criticized for creating in many people a general emotional blunting,” Roseman told PsyPost.
Though more studies are being conducted on psychedelic drugs like psilocybin, the research is still in its early phases.
“The major caveats are a lack of control group, a lack of SSRI group, and that the time point of investigation is only one day after the psilocybin session and not more than that. All of these caveats will be addressed in our next trial,” Roseman said.
Generally, psilocybin-assisted therapy involves only a few sessions, he noted.
“It is important to emphasize that psilocybin-assisted therapy is a model in which the patient is undergoing a deep psychological process in one or few psychedelic sessions, in which he might have an intense cathartic experience, or peak experience,” Roseman explained.
Patients receive a dose of psilocybin in a controlled setting while professionals are on hand to provide them with psychological support. The patients also typically receive counseling before and after each session, to help them prepare for and integrate their psychedelic experience.
“This is unlike antidepressants which are given as chronic pharmacological intervention with less psychological insights,” Roseman said.
The study, “Increased amygdala responses to emotional faces after psilocybin for treatment-resistant depression“, was co-authored by Lysia Demetriou, Matthew B. Wall, David J. Nutt, Robin L. Carhart-Harris.
