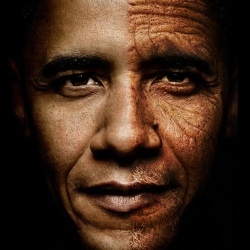
The goal is to reverse aging, not only in animals, but in humans. Reversal is essential, as significant age-related disruption has already occurred in most people due to changes in gene expression.
Gene expression patterns change with age. This influences the rate at which an individual ages, and also determines what senile disorders they are likely to contract. But innovative gene-editing methods based on a unique technology called CRISPR (clustered regularly interspaced short palindromic repeats) are now being successfully harnessed for use as an age-reversal therapy for humans.
In response to these breakthroughs, Life Extension magazine sent biogerontologist Dr. Gregory M. Fahy to Harvard University to interview Dr. George Church, who is a leading developer of cutting-edge CRISPR techniques. Here, Dr. Church explains remarkable opportunities for transforming human aging that may begin to unfold sooner than most have imagined.
Fahy: Using your most favorable pathway for intervention, how long will it take before a human trial might be possible?
Church: I think it can happen very quickly. It may take years to get full approval, but it could take as little as a year to get approval for phase one trials. Trials of GDF11, myostatin, and others are already underway in animals, as are a large number of CRISPR trials. I think we’ll be seeing the first human trials in a year or two.
Fahy: Can you say what those trials might be?
Church: I helped start a company called Editas that is aimed at CRISPR-based genome editing therapies in general. Some of those will be aimed at rare childhood diseases and others hopefully will be aimed at diseases of aging. We also have a company focused specifically on aging reversal that will be testing these therapies in animal and human models.
A discussion with Dr George Church on reversing cell aging by restoring youthful gene expression
Fahy: If aging is driven by changes in gene expression, then the ability to control gene expression using CRISPR technology could have profound implications for the future of human aging. Why do you think aging may be at least partly driven by changes in gene expression?
Church: We know that there are cells that deteriorate with age in the human body and that we have the ability to turn those back into young cells again. This means we can effectively reset the clock to zero and keep those cells proliferating as long as we want. For example, we can take old skin cells, which have a limited lifetime, and turn them into stem cells (stem cells are cells that can turn into other kinds of cells) and then back into skin cells. This roundtrip results in the skin cells being like baby skin cells. It’s as if my 60-year-old cells become 1-year-old cells. There are a variety of markers that are associated with aging, and those all get reset to the younger age.
Fahy: That’s fantastic. Does this mean that reversing skin cell aging in your face would allow you to rejuvenate your entire face?
Church: If you rejuvenate at a molecular level, it doesn’t necessarily mean that everything else rejuvenates. So, for example, if my face has a scar on it, it’s not going to necessarily reverse that (although theoretically it’s not out of the question). But we can reverse the tendency of your cells (and therefore of your whole body) to deconstruct when you reach your life expectancy.
How to Quickly Discover and Begin to Correct Currently Unknown Causes of Aging on the Gene Level
Fahy: If aging is driven by changes in gene expression and those changes in gene expression can be reversed, then we need to be able to find all of the important age-related changes in gene expression as quickly as possible. How can this be done?
Church: Gene expression results in each cell having specific RNAs and proteins, and these can be surveyed. You don’t necessarily have to define every single RNA in a particular cell to understand that cell, but you can, and we have in fact developed a new method to do this that allows us to see all of the tens of thousands of RNAs in a single cell at one time, and to see the RNAs in neighboring cells as well.
So now we can see how different cells relate to one another in context. This new method, called fluorescent in situ sequencing, or FISSEQ, allows us to count all the RNAs in a cell while simultaneously counting all of the RNAs in all of the cells it touches. Plus, we get the 3D coordinates for every RNA molecule in every cell.
Fahy: That’s unbelievable. How can you use this method to search for changes that are related to aging?
Church: Suppose there are two different kinds of cell, and we want to know what gene expression states make them different from one another. We can first compare the two cells using FISSEQ in order to determine the differences in gene expression between them. Next, we can pick specific differences we think cause the cells to be different cell types, and change the expression of those particular genes in either or both cells using, for example, CRISPR, and see if we can change one kind of cell into the other. Even if we don’t get it right the first time, we can take many guesses as to what the important RNAs are and just how much to tweak them until we do get it right.
The same principle can be applied to any pair of cells. By comparing old cells to young cells, we can find out what makes an old cell an old cell, and how to turn an old cell into a young one.
Fahy: Fantastic.
Church: One of the problems with studying development and aging is that it takes a long time. But if we know the epigenetic state of all these different cells, no matter how many years apart they are, it only takes a few days to reprogram a cell and duplicate the effects of decades of slow change in the body, or reverse those effects. So in principle we could turn a young cell into an old one or an old cell into a young one because the only difference between them is epigenetics, or gene expression.
Fahy: What other ways are there to identify powerful gene targets for intervention into human aging?
Church: There are basically four good ways to find key gene targets.
First, we can look at genes that underlie person-to-person variability in such things as low risk for viral infections, diabetes, osteoporosis, and so forth. The most extreme example here would be to compare normal people to super-centenarians, those who live to the age of 110 or older. They might have genes that are protective enough to find even with a small number of individuals, or even with a single individual.
There are hundreds of genes that have small effects, but then way out on the end of the bell curve is something like the myostatin double null mutant or human growth hormone over/under production. Genes that have gigantic effects and completely dominate the effects of small environmental and small genetic influences are the right kind of gene to look for.
The second way to find the best gene targets is to pick from discoveries made from basic studies like the GDF11 and TFAM that we talked about earlier.
A third way is to use a specialized highly genomic strategy, such as mutating thousands of genes one by one to see if any of these mutations block aging, or using the FISSEQ method we discussed earlier.
The fourth way to identify powerful gene targets is to compare closely related animals, one of which ages much more slowly than the other (like naked mole rats vs. rats).
No matter where you get your lead, you don’t have to worry about having too many hypotheses. Just use CRISPR to activate or inhibit that candidate gene and look for the biomarkers of aging reversal we discussed earlier. The idea is to see whether your change has an impact or not, and whether it acts synergistically with the other things that have been shown in the past to have an impact.
Fahy: So if we saw something unusual or provocative in super-centenarians, we could create the same change in, for example, a normal human cell line and observe whether the right longevity pattern emerged.
Church: Yes.
Fahy: I’ve been told by James Clement, who is being funded by the Life Extension Foundation to do collaborative work with you on the genetics of super-centenarians (See sidebar: Life Extension Foundation Funding of CRISPR Research), that you might even be able to take super-centenarian gene expression patterns and put them into mice and see if the mice age more slowly.
Church: Right. Our protocol will likely be to collect leads from the four different sources and try them out first on human cells. By going straight to human cells, we won’t get into the trap of spending years working on mice, which is rather expensive, only to find out that it doesn’t work in humans. We can actually do a cheaper and more relevant study in human cells, confirm them in mice, then test them in larger animals, and then in humans. I think that going from human cells to mice and back to humans is likely to save us time and money. Many human cellular testing systems are getting better and better, such as "organs on a chip" or organoids, which are getting to be more and more representative of in vivo biology.
The Feasibility of Applying CRISPR Technology to the Whole Body
Fahy: To reverse human aging, CRISPR technology will ultimately have to be applied in the whole body, and not just to cells in a test tube. How feasible is it to apply CRISPR technology in the intact body?
Church: Gene therapy can be based on either ex vivo manipulations, in which cells are removed from the body, genetically modified, and then put back into the body, or on in vivo (within the body) methods, in which, for example, a modified virus might be used to carry a gene package into many different cells in the body. Each of these methods has pros and cons.
There are viral and non-viral delivery systems that could be used to deliver CRISPR constructs and that will leave the blood vessels and go into the tissues. The delivery system could contain the CRISPR plus guide RNA plus the donor DNA (See sidebar: Gene Editing with CRISPR), or it could just comprise the CRISPR, guide RNA, and protein activator, and so on. But whether it’s a viral delivery or a non-viral delivery method, the total mass of gene editing devices that has to be delivered will have to be considerable. But there is no rush, you can deliver them slowly.
Fortunately, there are ways to manufacture biologicals that are dirt cheap. Things like wood and even food and fuel are all roughly in the dollar-per-kilogram range. If we could similarly make a kilogram of a viral delivery system and load it up with CRISPR, then it could become inexpensive enough to apply to the whole body.
Fahy: Yes, a kilogram would be plenty! So, the viral delivery system contains a gene for CRISPR, a separate gene for the guide RNA, etc. When it delivers these genes to the cell, the cell makes the resulting proteins and nucleic acids, and all of the components simply assemble all by themselves in the cell, is that right?
Church: Yes.
Fahy: Which is the best CRISPR delivery system?
Church: Adeno-associated viruses (AAV) are one of the favorite delivery systems right now because they can be nudged into going to tissues other than the liver (where many other delivery systems end up) more readily. This is an active field of discovery. It’s moving quickly, and the CRISPR revolution just made it an even more desirable field to study.
Specific Opportunities for Reversing Human Aging TFAM: Staying Energetic Indefinitely
Fahy: There are several very exciting stories in aging intervention these days. In 2013, the Sinclair lab at Harvard came out with the revelation that the aging of mitochondria (which are the producers of usable energy within cells) is driven in significant part by reduced levels of one particular molecule in the cell nucleus: oxidized NAD (NAD+).
The team showed that they could correct mitochondrial aging just by giving old mice nicotinamide mononucleotide (NMN), which is a vitamin-like substance that can be converted into NAD+, for one week. This resulted in phenomenal overall rejuvenation, including reversal of signs of muscle atrophy, inflammation, and insulin resistance. Now your lab showed that there is a very exciting gene engineering alternative involving TFAM (Transcription Factor A, Mitochondrial). Why is TFAM important, and what have you done with it?
Church: TFAM is a key regulatory protein that is in this pathway of NMN and NAD+. It allows cells to manufacture the NMN precursor on their own, so you don’t have to manufacture it outside the cell and then try to get it into the cell from outside. Ideally, you don’t want to have to take NMN for the rest of your life, you want to fix the body’s ability to make its own NMN and buy yourself rejuvenation for at least a few decades before you have to worry about NMN again. In order to accomplish this on a single cell level, we’ve used CRISPR to activate a TFAM activator, and we made it semi-permanent. (See sidebar: Gene Editing with CRISPR)
Fahy: With this technique, you were able to increase TFAM levels in the cell by 47-fold. This resulted in restored ATP levels, increased NAD+, and an increased NAD+ / NADH ratio. It also increased total mitochondrial mass and reversed several other age-related changes.
Church: Yes. We have a number of ways to measure mitochondrial function and age-related losses of those functions. When we activated TFAM, these changes returned to what you would expect of a younger cell state. And we built this anti-aging ability into the cell, so it’s self-renewing and eliminates the need to take pills or injections.
