A man who had been in a vegetative state for 15 years has shown signs of consciousness after neurosurgeons implanted a vagus nerve stimulator, challenging the belief that disorders of consciousness that persist for longer than 12 months are irreversible.
In a 2007 Weill Cornell Medical College study reported in Nature, neurologists found temporary improvements in patients in a state of minimal consciousness while being treated with bilateral deep brain electrical stimulation (DBS) of the central thalamus. Aiming instead to achieve permanent results, the French researchers proposed use of vagus nerve stimulation* (VNS) to activate the thalamo-cortical network, based on the “hypothesis that vagus nerve stimulation functionally reorganizes the thalamo-cortical network.”
After one month of VNS, a treatment currently used for epilepsy and depression, the patient’s attention, movements, and brain activity significantly improved and he began responding to simple orders that were impossible before, the researchers report today (Sept. 25, 2017) in an open-access paper in Current Biology.
For example, he could follow an object with his eyes and turn his head upon request, and when the examiner’s head suddenly approached the patient’s face, he reacted with surprise by opening his eyes wide.
“After one month of stimulation, when [electrical current] intensity reached 1 mA, clinical examination revealed reproducible and consistent improvements in general arousal, sustained attention, body motility, and visual pursuit,” the researchers note.
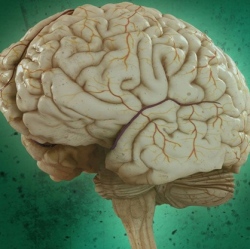
Brain-activity recordings in the new study revealed major changes. A theta EEG signal (important for distinguishing between a vegetative and minimally conscious state) increased significantly in those areas of the brain involved in movement, sensation, and awareness. The brain’s functional connectivity also increased. And a PET scan showed increases in metabolic activity in both cortical and subcortical regions of the brain.
The researchers also speculate that “since the vagus nerve has bidirectional control over the brain and the body, reactivation of sensory/visceral afferences might have enhanced brain activity within a body/brain closed loop process.”
The team is now planning a large collaborative study to confirm and extend the therapeutic potential of VNS for patients in a vegetative or minimally conscious state.
However, “some physicians and brain injury specialists remain skeptical about whether the treatment truly worked as described,” according to an article today in Science. “The surgery to implant the electrical stimulator, the frequent behavioral observations, and the moving in and out of brain scanners all could have contributed to the patient’s improved state, says Andrew Cole, a neurologist at Harvard Medical School in Boston who studies consciousness. ‘I’m not saying their claim is untrue,’ he says. ‘I’m just saying it’s hard to interpret based on the results as presented.’”
