People with untreatable cancers have had their immune system redesigned to attack their own tumours. The experimental study involved only 16 patients, but has been called a “leap forward” and a “powerful” demonstration of the potential of such technology. Each person had a treatment developed just for them, which targeted the specific weak spots in their tumour. It is too early to fully assess the therapy’s effectiveness and it is expensive and time-consuming.
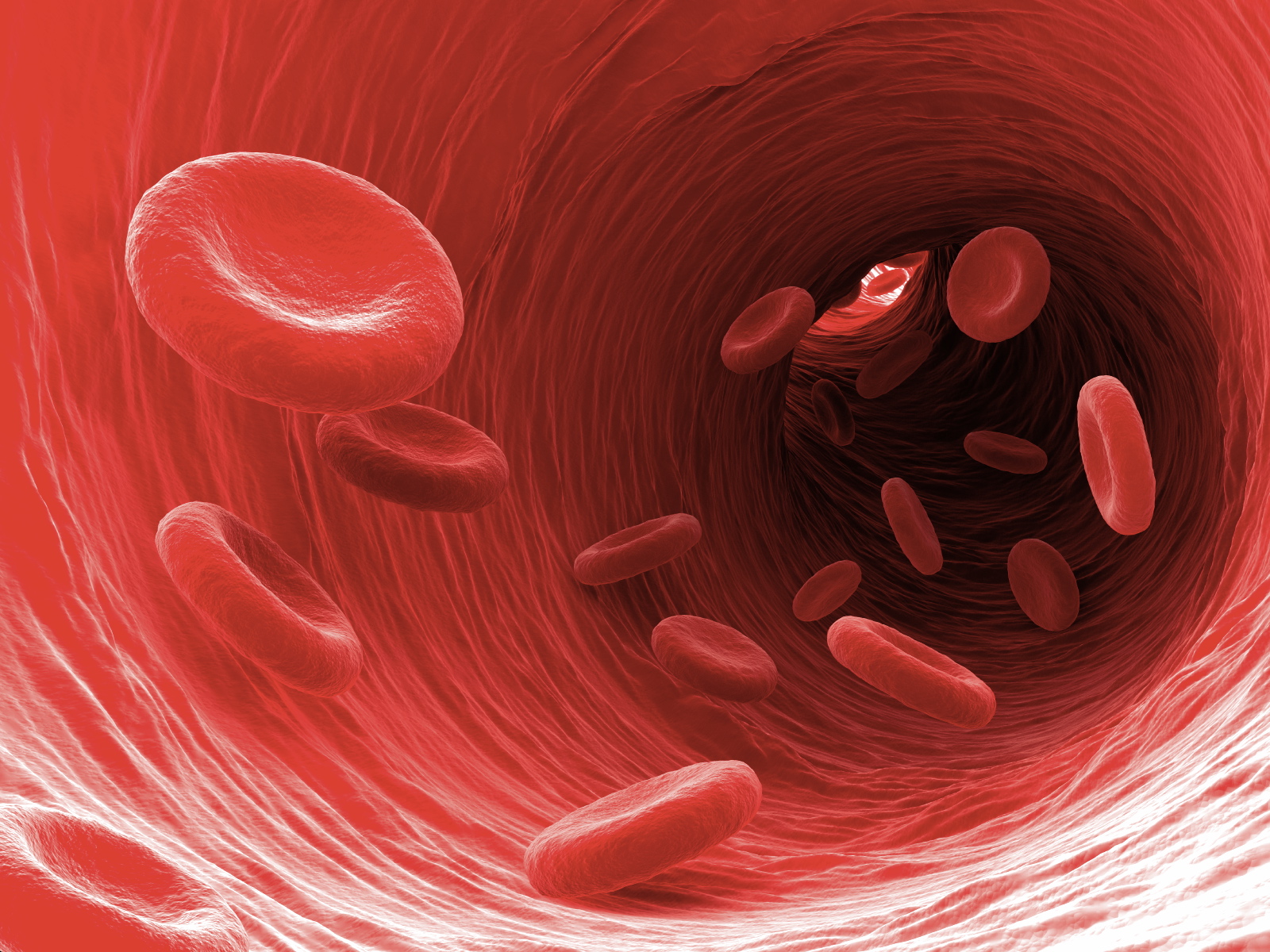
The work focuses on a part of the immune system called T-cells, which patrol the body and inspect other cells for problems. They use proteins – called receptors – to effectively sniff out signs of infection or deviant cells that have become cancerous.
Cancers can be tricky for T-cells to spot. A virus is distinctly different to the human body, but cancers are more subtle because they are a corrupted version of our own cells.
The idea of the therapy is to boost levels of these cancer-spotting T-cells. It has to be tailored to each patient as each tumour is unique.
This is how it works:
The researchers scoured patient’s blood for rare T-cells that already had receptors which could sniff out their cancer
They then harvested other T-cells that could not find the cancer and redesigned them
Their original receptors, which may find other problems or infections, were replaced with those from the cancer-searching T-cells
Finally, these modified T-cells were then put back into the patient to seek out the tumour
Transforming T-cells into a form that can hunt cancer requires considerable genetic manipulation to both remove the genetic instructions for building their old receptors, and give them the instructions for the new ones.
It was made possible by tremendous advances in the gene-editing technology Crispr, which acts like a pair of molecular scissors – allowing scientists to easily manipulate DNA. The researchers who developed Crispr won the Nobel Prize for Chemistry in 2020.
