Promising preliminary data from one of the first human trials testing the safety and efficacy of a CRISPR gene therapy has just been revealed. Although it is too early to evaluate long-term effects, the initial reports are impressively successful for two patients with severe genetic blood diseases.
Until February of this year, when pharmaceutical companies CRISPR Therapeutics and Vertex began a large global trial into a treatment called CTX001, no human outside of China had been officially treated with a CRISPR-based gene editing therapy.
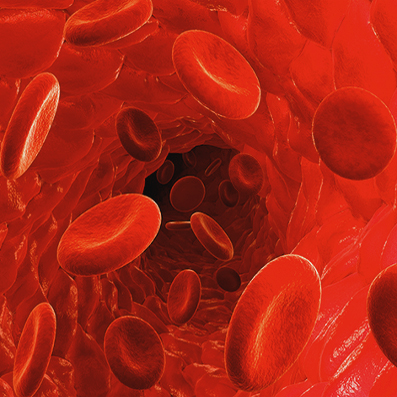
CTX001 was developed to treat two types of inherited blood disease, beta-thalassemia and sickle cell disease. Both conditions are caused by a mutation in a single gene and the treatment involves engineering a patient’s stem cells with a single genetic change designed to raise levels of fetal hemoglobin in red blood cells.
The newly announced data from the first two patients treated with CTX001 is nothing short of extraordinary. The first patient was treated with the CRISPR therapy at the beginning of 2019 for transfusion-dependent beta-thalassemia. The patient’s illness was so severe they required around 16 blood transfusions every year. Nine months after the single CTX001 treatment the patient was completely independent of the need for blood transfusions and their total hemoglobin levels were near normal.
The second patient, treated for sickle cell disease, demonstrated similar remarkable responses to the one-off gene therapy treatment. Four months after the CTX001 infusion the patient’s total hemoglobin levels had returned to normal and many of the disease symptoms had disappeared.
“We are very encouraged by these preliminary data, the first such data to be reported for patients with beta thalassemia and sickle cell disease treated with our CRISPR/Cas9 edited autologous hematopoietic stem cell candidate, CTX001,” says Samarth Kulkarni, CEO of CRISPR Therapeutics. “These data support our belief in the potential of our therapies to have meaningful benefit for patients following a one-time intervention.”
