In two decades, 3-D printing has grown from a niche manufacturing process to a $2.7-billion industry, responsible for the fabrication of all sorts of things: toys, wristwatches, airplane parts, food. Now scientists are working to apply similar 3-D–printing technology to the field of medicine, accelerating an equally dramatic change. But it’s much different, and much easier, to print with plastic, metal, or chocolate than to print with living cells.
“It’s been a tough slog in some ways, but we’re at a tipping point,” says Dean Kamen, founder of DEKA Research & Development, who holds more than 440 patents, many of them for medical devices.
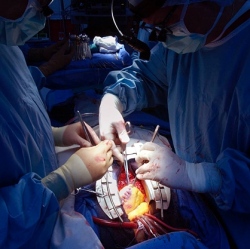
In labs around the world, bioengineers have begun to print prototype body parts: heart valves, ears, artificial bone, joints, menisci, vascular tubes, and skin grafts.
Three factors are driving the trend: more sophisticated printers, advances in regenerative medicine, and refined CAD software. To print liver tissue at Organovo, Vivian Gorgen, a 25-year-old systems engineer, simply had to click “run program” with a mouse. Honeycomb-shaped liver tissue is a long way from a fully functioning organ, but it is a tangible step in that direction. “Getting to a whole organ-in-a-box that’s plug-and-play and ready to go, I believe that could happen in my lifetime,” says Presnell. “I cannot wait to see what people like Vivian do. The potential is just out of this world.”
3D Printing is just the start
Lipson’s first printed meniscus (knee tissue) looked promising, when he showed it to knee-replacement surgeons, they deemed it too weak to withstand the body’s routine abuse. “As somewhat of an outsider coming in [to biology], my impression was ‘Okay, I’m gonna put the cells in the right place, incubate it for a while, and we’re gonna have our meniscus,’ ” Lipson says. “There is more to making a meniscus than just putting the cells there. Real menisci are actually pounded every day, all the time, and they shape up and become stiff. So the pounding that’s in their environment is actually very much a part of their growth.”
A printer that can dispense the right ink, in other words, is only the first step. Cells have specific requirements, depending on the tissue they’re destined to become. In the case of a meniscus, it might mean developing a bioreactor that can approximate pounding or use heat, light, or auditory pulses to stress the tissue into formation. “For some tissues, even the simple ones, we don’t even know exactly what it takes to make the tissue behave like a real tissue,” says Lipson. “You can put the cells of a heart tissue in the right place together, but where’s the start button?”
Tissue Scaffolds or no Scaffolds
Scaffolds provide tissues with mechanical stability, and they can be used to deliver genes and growth factors to developing cells. But, as in the case of polymers, they can introduce foreign materials into the body and cause inflammation. Cell types also respond differently to certain scaffold materials, and so the more complex the organ, the more complicated the necessary framework—and the more difficult to predict how the cells will migrate around it. As a result, not everyone believes scaffolds are necessary, including Gabor Forgacs, Organovo’s co-founder and a biological physicist at the University of Missouri.
Forgacs’s plan is to print an organ composed entirely of living human tissue and let it assemble itself. “The magic,” he says, “happens after printing has taken place.” Therein lies the biggest misconception about bioprinting: What most people think of as the finished product—the newly printed cellular material—isn’t finished at all.
At Missouri, Forgacs studied morphogenesis, the process that determines how cells form organs during embryonic development. By arranging cellular aggregates—tiny spheres containing thousands of cells—into a circle, his lab could watch them fuse and form new structures. The aggregates accomplish this by working together. A molecule on one cell causes a receptor protein on the cell membrane to change shape, tugging on the cytoskeleton of a second cell. A cascade of communication ensues, eventually reaching the nucleus and triggering a change in gene expression.
A grant from the National Science Foundation enabled Forgacs and his team to experiment with bioprinters instead of laying down aggregates by hand, and the technology transformed their research. “What had taken us days, we could do in maybe two minutes,” he says. Using a bioprinter, Forgacs proved that aggregates containing different cell types also fuse, without any human intervention or environmental cues.
